The vagus nerve is not your most well-known body part, but it’s certainly one of the most important. A newly approved application that affects the nerve gives hope to stroke victims who are working to recover use of an arm or hand.
The vagus nerve is one of 12 pairs of cranial nerves that send electrical signals between your brain and different parts of your head, neck and torso. You have one vagus nerve on each side of your body, starting at your brainstem and passing through your neck to your chest and abdomen. They carry signals between your brain, heart and digestive system and are a key part of your parasympathetic nervous system, which controls mind and body functions such as mood, immune response, digestion and heart rate.
Vagus nerve stimulators (VNS) have been used for a variety of treatments since 1998, but an updated application to treat stroke victims that was recently approved by the FDA has become an exciting option for stroke patients receiving physical therapy. Turns out that stimulating the vagus nerve in a particular way prompts the brain to rewire itself around the site of the stroke, helping to recover arm strength and movement.
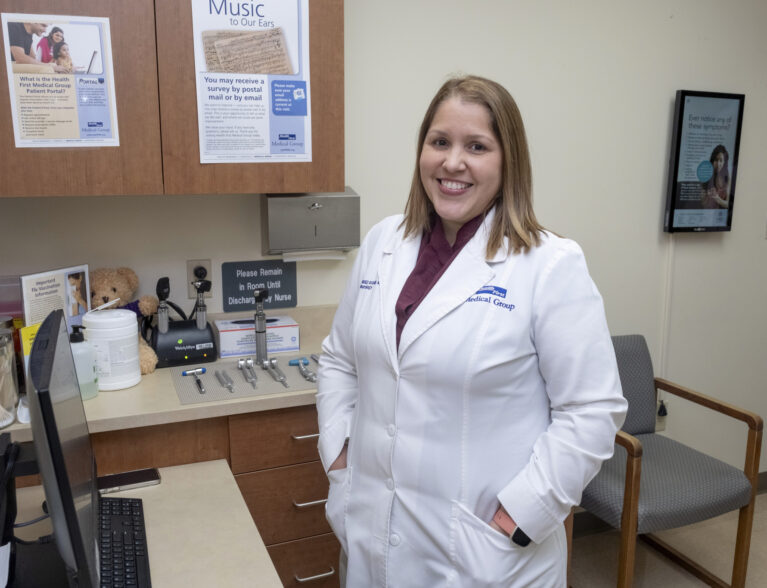
Dr. Lina Rodriguez Rosario, a neurologist at Health First’s Holmes Regional Medical Center, has been using VNS with epilepsy patients for five years and believes its expanded use to help stroke recovery is an important development. “The main difference for the new application is in the device itself,” she says.
In order to stimulate the vagus nerve, a small device that could fit in the palm of your hand is surgically implanted under the skin in the upper left chest area during an outpatient procedure. Patients are discharged the same day. After a one-week recovery from implantation, the stroke survivor continues in-clinic physical therapy.
During physical therapy, a therapist will use a wireless transmitter to signal the implanted device to deliver a gentle electric pulse to the vagus nerve while the patient performs tasks such as flipping a coin, shaking a hand or cutting food.
The pairing of exercise with vagus nerve stimulation releases neuromodulators that create or strengthen neural connections to improve upper limb function and increase the effect of physical therapy.
According to Mayo Clinic, where the stroke VNS is used, the stimulation device helps create new pathways in the brain as the patient performs exercises, which can help the patient regain arm and hand function faster than rehabilitation alone.
The device works by delivering stimulation the moment a patient is performing a rehabilitation exercise. Pairing these actions can help patients recover lost strength from stroke and, in many cases, regain function in their hands and arms. Nearly half the Mayo patients who used the therapy during the chronic phase of recovery had significant improvement in motor strength.
Dr. Rodriguez Rosario says that in addition to epilepsy, VNS stimulators are effective in treating depression and headaches. “It helps to reduce the need for pain medication,” she says, “and because it’s FDA-approved, it’s covered by most insurance.”
The treatment is not for everyone, however.
According to Cleveland Clinic’s website, you may not be a good candidate for VNS if you:
- Are pregnant.
- Have breathing problems, including asthma, sleep apnea, chronic obstructive pulmonary disease or other lung diseases and disorders.
- Have active peptic ulcer disease.
- Have insulin-dependent diabetes mellitus.
- Have only one vagus nerve.
- Have dysautonomias, which involves abnormal functioning of your autonomic nervous system.
- Are receiving other forms of brain stimulation.
- Have heart arrhythmias or other heart abnormalities.
Dr. Rodriguez Rosario says that a neurologist is usually the medical professional who decides if VNS stimulation is appropriate, with a neurosurgeon performing the relatively simple surgical procedure.
Dr. Lina Rodriguez Rosario is board-certified in Neurology and Neurophysiologic Monitoring by the American Board of Psychiatry and Neurology. She earned her Doctor of Medicine from Universidad Central del Caribe School of Medicine in Bayamon, Puerto Rico, did her internship in Internal Medicine at Hospital Universitario Ramon Ruiz Arnau in Bayamon, Puerto Rico, and her neurology residency with the University of Florida College of Medicine in Jacksonville. She completed her neurophysiology-EEG fellowship at the Medical University of South Carolina in Charleston. She is accepting new patients at Health First Medical Group – Gateway, 1223 Gateway Dr., Suite 2G, Melbourne: 321-312-3503.



