Cleveland Clinic Indian River continues to supply their surgeons with the latest technology to perform procedures with acute precision and accuracy. Such is the case with the advanced robotic-assisted bronchoscopy that is revolutionizing the way bronchoscopies are performed.
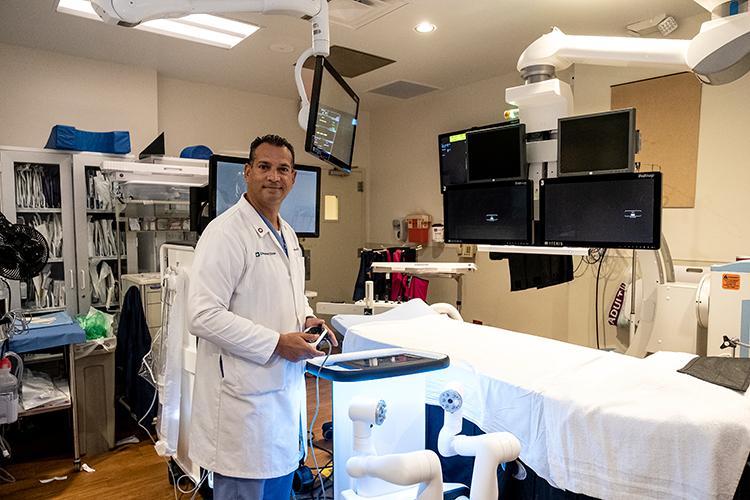
Pulmonologist Dr. Hermes Velasquez, who performed the first robotic assisted bronchoscopy at Cleveland Clinic Indian River Hospital this past July, told Vero Beach 32963 that “the advantages of using the robotic technique are threefold.
“First it allows us to navigate more precisely. Secondly, we get more range, which allows us to reach further into the bronchial tube. And thirdly, it is more stable and once we reach our targeted place we can anchor the device in that position, making it more advantageous to start the sampling process for biopsies.”
The American Lung Association defines bronchoscopy as a technique used to look at your air passages with a small camera that is positioned at the end of a flexible tube. The camera is connected to a video screen where your doctor can view photos of the air passages. The tube also has a small channel to collect tissue samples from your lung that can be used for disease diagnosis.
With a traditional bronchoscopy, the physician would manipulate the bronchoscopy tube with instruments controlled by his hands. With the new robotic technology, the physician still controls the instrument but is able to move the flexible bronchoscopy tube with more precision, enabling him to reach parts of the lung that may have been challenging to access with traditional bronchoscopy techniques.
While the physician is controlling the robotic system, a 3-D map of the patient’s lung is shown on the computer screen. The map allows the physician to see exactly where the tube is in the person’s lung and guides the physician to get to the nodule.
Robotic-assisted bronchoscopy is performed on eligible patients who are diagnosed with a lung nodule or lung mass and need to have a biopsy to determine that nodule is cancerous or not.
The outpatient procedure is done under general anesthesia. On the day of the procedure a CT scan will be taken of the chest with special protocol which will serve as the mapping tool. That specific picture of your chest is recorded on a CD, which in turn is placed in the robotic software. The software will identify lesions in the CT scan and create a visual path for the physician to follow.
Once the patient is sedated, a flexible tube is inserted through the endotracheal tube. The catheter is then manipulated by a controller operated by the physician. The physician follows the designated path that is mapped from the CT scan of your lungs leading directly to the nodule.
“The procedure is based on electromagnetic navigation,” Dr. Velasquez said. “A special sensor is placed in the periphery of the patient. These sensors guide the robot with our movement to the precise spot where the robot identified the nodule. We then use additional imagining guidance … Biopsy tools are then used to take samples from the nodule. Using these combined tools gives us precise accuracy.
“We have a pathologist on site, so as we get the samples, we can have the pathologist look at them on a slide and in a matter of minutes I can have the input that yes, it is compatible with cancer, or no, it is not cancerous but may be compatible with other inflammatory conditions.
Or he may say that all he sees is good lung; then the robot will help to guide me to a different position so I can extract a better sample. This process is called rapid on-site evaluation.”
If the patient has two or three lesions on the same side of the lung, they can all be biopsied at the same time. Samples cannot be taken from both sides of the lung for safety reasons, but the patient can come back for the procedure on the other side at a later date. There is no limit on how many times a patient can undergo the procedure.
“Our goal is to detect lung cancer early in the game and ultimately save lives,” Dr. Velasquez said. “Lung cancer is curable if caught early, but unfortunately most lung cancer is discovered past the curable stage. That’s why it’s so important to get a CT lung cancer screening to make sure there are no lesions. By doing so we can attack the cancer in its earliest stages.”
Since 80 percent of all lung cancers are smoking related, the CDC recommends yearly screenings for anyone over the age of 50 who currently smokes or has quit smoking in the past 15 years and has a 20-pack year smoking history. To determine your smoking history, multiply the number of packs of cigarettes smoked per day by the number of years smoked.
Dr. Velasquez completed his medical education at Universidad del Aulia in Maracaibo, Venezuela, and his internship and residency in internal medicine at Jackson Memorial Hospital/University of Miami. He served a fellowship in pulmonary medicine at Jackson Memorial Hospital in Miami.
Dr. Hermes Velasquez can be reached at his office at the Cleveland Clinic Indian River Hospital Health and Wellness Center, 3450 11th Court, Vero Beach, or by calling 772-794-5800.



