It’s not an over-dramatization to call an abdominal aortic aneurysm a “silent killer.” When a weakness in the aortic wall balloons to the point of rupture, death can – and usually does – occur immediately, with as high as a 90% death rate associated with a rupture.
Fortunately, says Sebastian vascular surgeon Dr. Hadi Shalhoub, test now exist to identify an aneurysm, the “ballooning” of an artery caused by weakening of the arterial wall, which can occur and expand over time with no warning signs. Major technological advances have been made in the surgical procedures to repair it.
To be sure, aneurisms are still a serious problem. Even in the case of a “contained rupture,” when death is not immediate, a severe drop in blood pressure and loss of consciousness occurs. Of patients hospitalized under those conditions, on average only one in five will leave the hospital alive.
More than 15,000 deaths from abdominal aortic aneurysms (AAA) occur annually in the U.S. The prevalence increases with age (80% of his AAA patients are over 65), and other risk factors, he said, include smoking, “familial predisposition,” being overweight, and having high blood pressure. The ailment strikes women less frequently than men.
The good news, says Dr. Shalhoub, is that a simple screening, a non-invasive ultrasound procedure, can detect an aneurysm, which can then be repaired if it’s over 5 centimeters, or tracked if it’s under. The screening can take place in the doctor’s office or the hospital and in the last two years Medicare has begun to pay for screenings for those 65 and up.
Given the deadly risk, Shalhoub urged people who qualify for Medicare as well as those of any age with any of the risk factors to make the screening a priority.
Previously, an AAA was repaired with a major invasive surgical procedure that would take about two hours. An incision was made from the sternum to the pubic bone and the organs were moved aside to access the aorta, the largest artery in the body that extends from the heart’s left ventricle down to the abdomen and distributes oxygenated blood to the body through the circulatory system. It lies along the posterior wall of the abdomen.
In the old operations, the aortic blood flow then had to be interrupted to the pelvis and lower extremities using clamps, after which the damaged section of the vessel was replaced with a polymeric material. The patient must then spend five to seven days recovering in the hospital, including two days in the ICU, with a tube from the nose to the stomach and a catheter in the bladder. With this major, invasive procedure, there was significant blood loss and, with the extended hospital stay, greater risk of exposure to infection.
Today however, other options have been developed which reduce the risks of invasive surgery for many patients. EVAR or endovascular aneurysm repair, is a minimally invasive alternative, in which a stent is deployed into the aneurysm inside the aorta through two small incisions on either side of the groin, providing a permanent, alternative conduit for blood flow, excluding the aneurysm “balloon” from flow and pressure, thus preventing a rupture without surgically opening or removing part of the aorta.
The latest minimally invasive procedure, Shalhoub explained, is PEVAR, or Percutaneous Endovascular Aneurysm Repair, which requires only a small (.5cm) puncture in both legs near the groin, to place the stent and bypass the aneurysm, using polymeric material. These small punctures can be addressed with a single suture or potentially covered by a single Band-Aid.
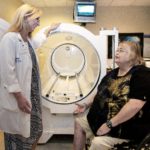
Shalhoub uses a fluoroscope for continuous observation of the stent deployment. PEVAR, he said, offers the least exposure to infection, the least blood loss, no risk of hernia, adhesions or scar tissue, local or regional rather than general anesthesia and less post-operative pain.
“The patient can leave the next day,” Shalhoub explained. “No tubes are necessary.”
Additionally, the procedure itself takes about half as long. Shalhoub believes he is currently the only vascular surgeon in the area who uses PEVAR, which he performs at Sebastian River Medical Center.