As if parents didn’t have enough to worry about, the Mayo Clinic, Johns Hopkins All Children’s Hospital and local dentist Dr. Jenna Schwibner of Dental Partners of Vero Beach all agree obstructive sleep apnea is something that should be added to every parent’s and grandparent’s check list.
And maybe even to their “worry” list.
The Mayo Clinic says “pediatric obstructive sleep apnea is a sleep disorder in which your child’s breathing is partially or completely blocked repeatedly during sleep. The condition is due to narrowing or blockage of the upper airway during sleep,” and the consequences can be dire.
“Early diagnosis and treatment,” says the Clinic, “are important to prevent complications that can affect children’s growth” and health.
Indeed, it goes on to say “children with sleep apnea might perform poorly in school; have difficulty paying attention; have learning problems; have behavioral problems, poor weight gain or be hyperactive.”
Or, as the American Sleep Apnea Association puts it, “the evidence is steadily growing that untreated pediatric sleep disorders, including sleep apnea, can wreak a heavy toll,” on any child.
The ASAA points out that “as many as 25 percent of children diagnosed with attention-deficit hyperactivity disorder may actually have symptoms of obstructive sleep apnea and that much of their learning difficulty and behavior problems can be the consequence of chronic fragmented sleep.”
Hopkins is equally blunt when it says “sleep apnea in children may be difficult to recognize and diagnose and may show up as daytime behavioral problems or bedwetting,” and it adds “there are differences between pediatric obstructive sleep apnea and adult sleep apnea.
“While adults usually have daytime sleepiness, children are more likely to have behavioral problems.”
Schwibner says “we’re seeing 90 percent of kids showing one kind of sign or symptom of sleep-disordered breathing.”
She adds that does not mean 90 percent of children have obstructive sleep apnea, but the statistic does draw attention to some caution flags; one of the most common of those flags is persistent mouth-breathing.
“What we’re seeing,” Schwibner continues, “is that nasal breathing is extremely important; that’s well documented. Everybody, all the doctors, know that the nose is the important filtration system of the body. The nose purifies, moistens and warms the air as we are breathing it. So, if we breathe it through our nose, we’re getting proper filtering. What happens when we mouth-breathe is all those toxins are going into our tonsils and adenoids causing [them] to become really swollen because our nose isn’t filtering it.”
And, moving on to a more traditional area of dental expertise, Schwibner adds, “we were taught in dental school that some mild grinding of the teeth in kids is just something normal that you grow up and you grow out of. But now they’re showing that 70 percent get worse and only 30 percent will self-correct. So [most of those teeth-grinding children] are not just going to get better on their own.”
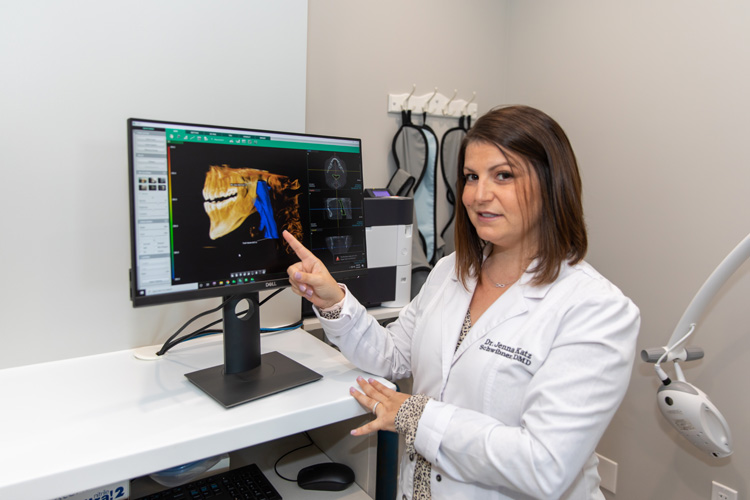
While pediatric sleep apnea is clearly a hot-button issue for Schwibner, she says “when it comes to sleep apnea, I’m not diagnosing it.” She is, however, ready, willing and able to help pediatricians, otolaryngologists and ENTs screen for it.
“One of my plans is to partner with a lot of the [pediatric] physicians in town, because this isn’t something that is well known. We have great pediatricians in town, and I have some great relationships with them. So, part of our goal is to do some educational evening events. Once they know more about it, they’re going to start seeing these things” in their pediatric patients.
To bolster her current effort to spread the word about pediatric sleep apnea, Schwibner says she’s planning to open a new, separate office in June of this year aimed at children.
In Schwibner’s eyes, a parent’s best bet is to talk with their child’s pediatrician or otolaryngologist if they notice their child snoring, tossing and turning in their sleep or consistently breathing through their mouth instead of their nose.
She can provide parents a sleep questionnaire to fill out or help arrange a take-home sleep study. She can also provide orthotic devices a child can wear at night that help train them to breathe through their nose.
“As long as they don’t have an anatomical reason why they can’t breathe through their nose,” says Schwibner, “it’s going to retrain them to breathe properly through their nose,” and that may just be the key to reducing obstructive sleep apnea in children.
Dr. Jenna Katz Schwibner is the practice owner at Dental Partners of Vero Beach. Her main office is at 3790 7th Terrace, Suite 201. The phone number is 772-569-4118. The office geared for young patients is scheduled to open in June.



