When the Centers for Medicare & Medicaid Services (CMS) shifted the way it pays medical providers for hip and knee replacements last April, some pundits predicted the number of those procedures would start to plummet.
They didn’t.
In fact, according to Lisa Cox, director of medical and surgical services at the Sebastian River Medical Center, the number of these procedures at SRMC has actually risen some 38 percent.
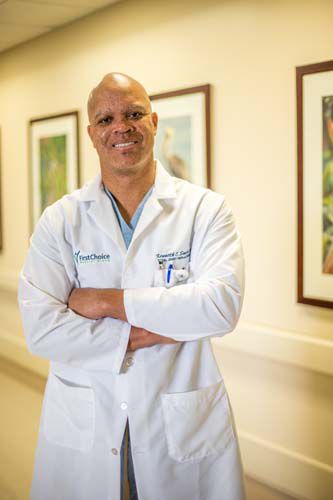
Contributing factors to that upswing likely include the hospital’s implementation of what’s known as the “Marshall Steele Program” and the growing practice of Melbourne-based orthopedic surgeon Dr. Kenneth Sands, who performs his surgeries in Sebastian.
Marshall Steele is a renowned orthopedic surgeon in Annapolis, Maryland. He developed a nationally-recognized surgical pathway for total joint patients from pre-op through surgery to post-op and rehabilitation.
Acquired by Stryker Performance Solutions in 2011, Steele’s patient-centric approach has since been adopted by healthcare facilities nationwide.
“Every hospital,” wrote Steele in a 2016 article on MedCitynews.com, “must find ways to improve quality, patient experience, collect outcomes while at the same time lowering overall costs. This includes managing costs after patients leave the hospital.”
That sentiment became doubly important when the new Comprehensive Care for Joint Replacement rules were issued.
In a nutshell, the CCJR makes hospitals responsible for the care quality as well as the cost of joint replacements for a full 90 days after a patient is discharged.
As U.S. News & World Report says, “Doctors, hospitals, rehab centers, therapists, home health agencies and other providers will continue to get their regular reimbursements from Medicare, but at the end of the year, hospitals will be held accountable for the total cost of care over the 90-day period.” If those costs exceed Medicare’s targeted total, hospitals will have to pay back many of the dollars they received from Medicare.
Sands says he has no problem with SRMC’s implementation of the Marshall Steele Program.
“It hasn’t encumbered me in any way,” says the man who spent more than a dozen years as a U.S. Army orthopedic physician and director of the Army’s Adult Joint Reconstruction program at the William Beaumont Army Medical Center in El Paso, Texas.
“Actually,” he says, “if anything, it adds to the program.”
Sands has built his reputation here in no small part by being the first – and the only – orthopedic surgeon in Florida to adopt an “anterior cruciate ligament or ACL-sparing” approach for knee replacements.
In the most commonly performed total knee replacements – both here and across the country – one of the first things that happens is that the ACL is cut away.
Sands believes that summarily removing a healthy ACL can be a big mistake. “When you preserve the ACL,” Sands says, “the [replacement] knee is being driven by the natural ligaments and it feels more natural.”
The U.S. National Library of Medicine backs up Sands’ contention, stating that knee replacement procedures “which retain the ACL provide relatively normal knee kinematics and favorable knee function compared with conventional knee replacement surgeries which sacrifice the ACL.”
And while Sands goes out of his way to credit “better anesthesiology and better implants” as contributing factors to better results, the fact remains that his preferred procedure has also contributed to the demand for his services.
When it comes to hip replacements, Sands is also taking a path less traveled.
While up to 95 percent of hip replacements in this country are currently being done using either a “posterior” approach, which involves a 4-to-6-inch incision in the buttock, or with a “lateral” approach that requires muscles in the hip area to be partially or completely detached, Sands – who says he’s “always looking for a better way” – favors a third technique.
Sands uses what’s called an “anterior” approach to hip replacements – in part because it’s the most direct route to the hip bone and also because it avoids any division or cutting of the body’s existing muscles.
Sands sums up his stance in three simple sentences.
“On the knee side we spare the ACL and all the ligaments. On the hip side, we spare cutting any muscles. The less invasive we are, in theory, the better it is for the patient.”
So, that 38 percent increase in knee and hip procedures at SRMC may well be tied, at least in part, to both SRMC’s implementation of the Marshall Steele Program and to Sands’ innovative surgical techniques.
Dr. Kenneth Sands has offices in Melbourne at First Choice Medical Group at 709 S. Harbor City Blvd. In Viera his offices are in the Delorenzi Orthopedic Center, 7000 Spyglass Court. In Vero Beach he is at 1715 37th Place. The phone number for all three locations is 321-725-2225. Lisa Cox can be reached at the Sebastian River Medical Center joint center at 772-589-3186.



