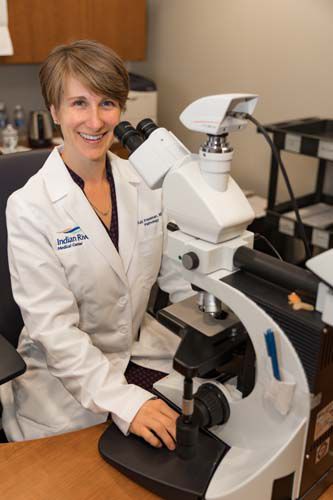
Dr. Kali (pronounced Kay-lee) Freeman, hematopathologist and medical director at the Indian River Medical Center’s pathology department, doesn’t have the most glamorous job in medicine.
But without Freeman and her staff of about 50, much of what the hospital does for its patients would come to a screeching halt.
So, what exactly are hematopathologists and what makes them so essential?
The American Association of Medical Colleges calls hematopathologists like Freeman “truly the doctor’s doctor, because they are board-certified in both clinical and anatomical pathology,” and it says “they form the basis of every physician’s thinking about the patient.”
Freeman puts it even more simply: “We’re the doctors that patients don’t see. We don’t go for the glamor. We like to stay in the back.”
“The lab,” Freeman continues, “is behind the scenes in the hospital. But without the lab, the hospital would be unable to function. Every time you get your blood drawn, a CBC, chemistry, or they check your white cells or your red cells, that’s all done here in the lab.”
Pausing only briefly, the diminutive Freeman adds, “Any time you have a biopsy or a surgery and something is removed, it comes to us and we’re the ones to come together with the clinician and make the diagnosis that helps you to get the right treatment.”
It takes a special kind of treatment-finder to spend the bulk of her day examining blood, urine, sputum or phlegm, spinal fluids, pleural fluids from the lungs, belly fluids, joint fluids, bone marrow and – yes – even feces.
On top of all that, various tissues, organs and tumors also fall into Freeman’s domain.
All of which, according to the Johns Hopkins Medical Library, requires “advanced skills in clinical chemistry, biology, toxicology, hematology, immunology, serology and microbiology.”
UCLA Health goes even further, saying those skills are “a vital part of the study and treatment of disease,” and states they are “closely affiliated with all the surgical specialties, internal medicine, dermatology, neurology, radiology, radiation therapy and medical oncology.”
In Freeman’s case, that’s a lot of medical sub-specialties all rolled into one petite and highly enthusiastic package.
She comes by it naturally. “My interest [in pathology] initially began because my mom had worked in the lab in a small community hospital where I grew up in Minnesota,” explains Freeman. “Being a pathologist was always in the back of my mind.”
“And then, throughout medical school, I enjoyed every rotation, actually. I enjoyed surgery, OB-GYN, pediatrics, everything. But when I did my pathology rotation I was just … I loved it! And at the end of the rotation I said, ‘Oh, I want to keep doing that. I want to do more of that.’”
Freeman’s enthusiasm becomes almost incandescent when asked about the opportunity to work with Dr. Suzanne Kirby, the newly arrived medical hematologist and oncologist at the Scully-Welsh Cancer Center next door.
“She’s wonderful,” beams Freeman. “I’m really excited. That’s one of the things we really want to do is grow the hematology program with leukemia and lymphoma. That’s my specialty and it’s her specialty. We’ll make a great team.”
“She’ll perform a bone marrow biopsy,” Freeman says, “[and then] I’ll evaluate it and perform all the molecular markers, the cytogenetics, and we can do next-generation sequencing, flow cytometry, all of these things to evaluate the cells in the milieu of the bone marrow to let her give the best possible treatment to the patient. We can really serve the people in the community.”
That, however, is not all that feeds Freeman’s drive. The recent addition of a “slide scanner” may not sound like something to get all that excited about, but when Freeman says “this is something that’s kind of cool,” a further explanation seems in order.
“In the same way that radiology used to actually be on film and now everything is digitized,” Freeman explains, “we’re slowly moving that way in pathology. Right now everything is still on [glass] slides. But we have a slide scanner, so we can digitize all of these images. We’re exploring the ability to do consultations and second-opinion consultations and even the possibility of making primary diagnoses on digital slides. [We] could call a pathologist who’s on vacation in the Bahamas or Hawaii or wherever, and ask them, ‘Hey, can you look at this?’’
It’s something, Freeman says, that’s already being done in Europe and Canada.
So while patients at IRMC may never see Freeman during their hospital stay, she almost certainly will see at least some part of them while helping the attending physician diagnose and treat their problems.
Dr. Kali Freeman is a practicing hematopathologist and the medical director of the Indian River Medical Center’s pathology department.



