There aren’t many diseases that have been newly identified in recent decades, but one with a tongue-twister of a name – eosinophilic esophagitis – falls into this category, and is now considered a major cause of digestive system illness.
Eosinophilic esophagitis (EoE) is a condition in which there is a build-up of white blood cells – eosinophils – in the lining of the esophagus. This build-up is a reaction to food, allergens or acid reflux, and can damage the esophageal tissue, resulting in difficult or painful swallowing, nausea and vomiting.
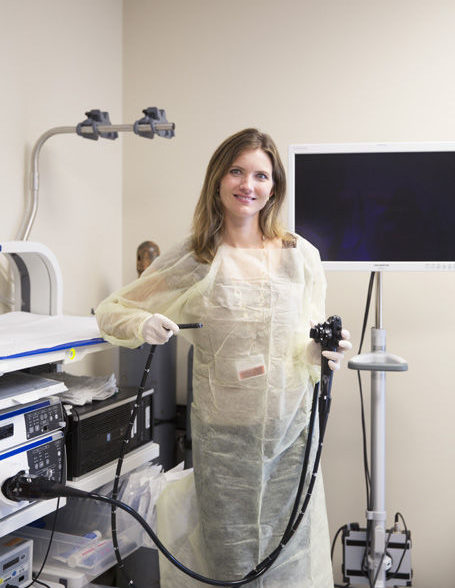
Dr. Ashley Canipe, an interventional gastroenterologist affiliated with Indian River Medical Center, says, “EoE is an immune-mediated condition, meaning the immune system is not attacking itself, but is reacting in a hyper-sensitive way to what it sees as an attack.” This hyper-sensitivity causes the white blood cells to flood into the esophagus, causing the damage and symptoms characteristic of the condition.
Katie Narracci is the daughter of seasonal barrier island residents Brian and Sue Keller. She has suffered from EoE for 20 years – about once a week, food gets lodged in her esophagus – but her diagnosis came just last year. Previously, doctors thought her problems were caused by a stricture (narrowing) of her esophagus, and treated her – unsuccessfully – by using various dilation techniques.
It’s not unusual for people with EoE to have asthma, food allergies, environmental allergies (Narracci has seasonal hay fever), eczema or chronic respiratory disease.
The disease is more common in males than in females; other risk factors include living in a cold or dry climate, and a family history of EoE. It was first thought to be a childhood disease, but is now known to affect adults as well. In fact, the average age at diagnosis is between ages 30 and 50 (Narracci was in her mid-20s when her symptoms began).
There is ongoing research on EoE, and scientists have recently identified a protein called “calpain 14” that may be the cause of the tissue damage that is characteristic of the disease. This is an important finding, as it can lead to treatments that control the activity of this protein and therefore prevent EoE from developing.
Doctors used to think that EoE symptoms were caused by gastroesophageal reflux disease (GERD), but it is now recognized as a unique condition, with distinct and separate causes. Vero’s Dr. Canipe says the two conditions can mimic each other, and even co-exist, and that ruling out GERD is an important step in the diagnostic process. “We’ll prescribe an acid blocker, such as a proton pump inhibitor,” she says. “If the symptoms go away, it’s most likely GERD.”
The only way to know for sure that a person has EoE is by an endoscopy and biopsy of the esophagus. An endoscopy is a non-surgical procedure that uses a flexible tube with a light and camera attached to allow doctors to see what’s happening in the esophagus. During the procedure, tissue samples are taken and later analyzed.
EoE is a chronic relapsing condition, and most people will require ongoing treatment to control their symptoms. This includes identifying which foods might produce the flood of white blood cells into the esophagus. Dr. Canipe advises her patients to follow what is called the “Six Food Elimination Diet,” in which milk, eggs, soy, wheat, peanuts/tree nuts, and fish/shellfish are avoided for three weeks or so and then gradually re-introduced into the diet, one by one, to see if symptoms reappear or worsen.
The medication of choice for EoE is a steroid, taken orally. Steroids may decrease the buildup of the white blood cells in the esophagus, reduce the inflammation, and allow the esophagus to heal. If steroids don’t work, and the esophagus becomes extremely narrowed, a dilation technique may be used.
Narracci is now treated with a twice-daily steroid inhaler; unfortunately, it has not reduced the frequency of her EoE occurrences. She has learned to live with the condition, and most of the time she can dislodge the stuck food by forcing herself to vomit. Once her esophagus is cleared, she feels fine and can continue eating. There are occasions when her technique does not work, and she must visit an ER or urgent care clinic for help.
In the past decade, there has been a significant increase in the number of people diagnosed with EoE, and it’s estimated to affect nearly 2 million people in the United States. The reasons for this increased prevalence are somewhat controversial; it is not known if there are really more cases or simply more awareness by doctors of the condition. Some studies suggest that the incidence of EoE is increasing in parallel with the increase in asthma and allergic conditions. “There is a definite environmental component,” Dr. Canipe says.
Symptoms of EoE should not be ignored. Dr. Canipe says people who can swallow, but only with difficulty, should contact their primary care physician, who may put them in touch with a gastroenterologist. “Some people with EoE get what’s called an impaction, in which food is so stuck that the person can’t even swallow their own spit,” she says. “In those cases, it’s important that they go immediately to the ER.”
EoE, especially if untreated, can lead to scarring and narrowing of the esophagus, making it even more difficult to swallow and more likely that food will get stuck. Perforation or tears in the esophageal lining tissue can also occur, especially in cases of an impaction.
Dr. Canipe’s office is located at 3745 11th Circle, Suite 101 in Vero Beach; the office phone is 772-299-3511.



