If you’re over 50, the odds are pretty good you’re already carrying a bacteria in your belly that may just give you an ulcer. About two thirds of the people on this planet do. If you also happen to pop an extra few aspirins each day to deal with arthritis or assorted other aches and pains, you may be throwing fuel onto a potential fire.
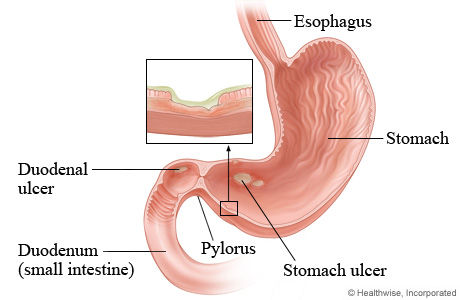
According to the National Institutes of Health, a particularly nasty strain of bacteria known as Helicobacter pylori or H. pylori is now recognized as the leading cause of both gastric and duodenal ulcers. (Ulcers in the stomach are called gastric ulcers. Ulcers in the upper area of the small intestine, or duodenum, are called duodenal ulcers. Collectively they’re often referred to as peptic ulcers.)
About two-thirds of the world’s population carries H. pylori and in the United States, it is found more often in older adults than in any other age group, which makes Vero’s senior-heavy population especially vulnerable.
Even in the healthiest people there are about 100 trillion bacteria present in the digestive system. Those “friendly” bacteria aid in the metabolism of nutrients and help get them into the bloodstream. H. pylori, however, is not a friendly bacteria.
Simply having H. pylori in your digestive system does not guarantee ulcers but approximately four million Americans do suffer from them, and one in 10 people are likely to develop one. Not coincidentally, H. pylori is found in more than 90 percent of all duodenal ulcers and 80 percent of stomach or gastric ulcers. The American Gastroenterology Association says ulcers are the most common form of stomach disease and they, too, cite H. pylori as the leading cause of these painful ailments.
Surprisingly, doctors and medical researchers didn’t even know this acid-loving strain of bacteria existed until 1982. For decades prior to that, spicy or especially acidic foods along with stress were considered to be the primary culprits in causing ulcers.
As to popping those extra aspirin tablets, the U.S. National Library of Medicine says research now shows that the over-use of nonsteroidal anti-inflammatory drugs — such as aspirin and naproxen products with trade names that include Aleve, Anaprox and Naprosyn — as well as ibuprofen products, including Motrin, Advil and Midol, can also cause or exacerbate the development of ulcers.
Dr. Mauricio Munoz, an internal medicine specialist here at Indian River Medical Associates, agrees. “Absolutely,” he exclaimed, “the more of those drugs you take, the greater your chance of developing ulcers.”
Even those so-called “safety-coated” aspirins can be an unintended sucker-punch to the gut for a stomach already fighting an H. pylori infection. The H. pylori bacteria excrete a substance that weakens both the stomach and the duodenum’s protective mucous barriers and excessive painkiller use, says Munoz, doesn’t help. In fact, those pills can sometimes cause an ulcer on their own or they can help finish off the job H. pylori may already have started creating actual holes in the lining of both the stomach and duodenum.
That’s what ulcers are: holes in the lining of the upper part of the gastrointestinal tract. Dr. Munoz reports that he, himself, saw as many as one or two ulcer cases every week while working at the hospital here in Vero.
Compounding matters is the fact that with advancing age, the valve between the stomach and duodenum sometimes relaxes and allows excess bile (a compound produced in the liver to aid in digestion) to seep into the stomach and further erode its lining leading to that burning, gnawing abdominal pain that so many will suffer from at some point in their lives.
Big or small, the stomach is a pretty hostile environment for just about everything except, unfortunately, H. pylori. The human digestive system is simply swimming with the acids that help in digestion and those acids are as about as toxic and corrosive as car battery acid. Once H. pylori or those anti-inflammatory drugs or a combination of the two have weakened the natural protective barriers, erosions or sores can develop and those erosions will eventually create an ulcer. If left untreated ulcers can lead to still more serious problems including anemia, profuse bleeding and, as Dr. Munoz points out, “a high risk of stomach cancer.”
There are a wide variety of symptoms associated with stomach or duodenal ulcers and the severity of the symptoms depends largely on the severity of the ulcer. The most common symptom is a burning sensation or pain in the area between the chest and navel. Normally, the pain is more intense when the stomach is empty. That pain can last for just a few minutes or it can go on for hours. Other common symptoms include unexplained weight loss; not wanting to eat because of pain; nausea; vomiting blood or material that looks like coffee grounds; burping and frequent heartburn.
Diagnosing ulcers can be simple or it can be fairly complex. A review of the patient’s medical history along with symptoms and a review of any prescription or over-the-counter medications currently being taken is the usual starting point. To rule out H. pylori infection, a blood, stool, or breath test may be ordered. Other tests and procedures might include a barium x-ray or an endoscopy in which a thin, light-emitting tube is inserted through the esophagus and into stomach and small intestine looking for signs of ulcers. In older patients or in those experiencing unusual bleeding, an endoscopic biopsy may even be ordered. In this procedure a small piece of tissue is removed and sent off for further analysis.
Once diagnosed, treatments will vary depending on the cause of the ulcer. The good news is that if H. pylori is detected, it can be fairly easily dealt with through a course of oral antibiotics. For mild to moderate peptic ulcers, many doctors will rely on drugs known as H2 blockers to prevent the stomach from making too much acid and giving the wound a chance to heal on its own. Even over-the-counter products such as Pepto-Bismol may be employed to protect the lining of the stomach and small intestine. In severe or recurrent cases, however, surgery may even be required.
There are also scores of “holistic” or “natural” remedies being marketed for ulcers. Dr. Munoz says he’s personally “open-minded” about many of those treatments, even pointing out that extracts from the aloe vera plant have shown some potentially promising initial results. However, he then sternly warns anyone wanting to try such remedies to check with their doctor before ingesting anything. “These products,” he points out, “have not been tested and don’t have FDA approval so patients should talk with their doctor first.”
Put another way, if you already have a stomach problem, the last thing you should do is swallow something that just might do more harm than good.
Dr. Mauricio Munoz is with Indian River Medical Associates at 1155 35th Lane, Suite 201, Vero Beach. 772-794-3364.



