Edwina DiPietro of Vero Beach used to play four-hour rounds of golf with the girls, three times a week, with the focus, of course, being on landing the ball into the cup. Eventually, her fixation became more about where the restrooms were located along the course.
That’s because DiPietro didn’t know when she might have an embarrassing moment of leakage, or urinary incontinence while playing. So, she eventually gave up playing altogether – except with her husband, who was aware of her situation. She also gave up travelling, much shopping and her daily five-mile walks.
“It impinged on my life,” DiPietro said of her sudden bout with incontinence of the bowels and bladder after back surgery in 2009. “It was a constant problem.”
DiPietro went from doctor to doctor to get the situation under control and although no doctor was able to tell her why incontinence crept up on her, she was able to get treatment at Urologic Wellness Center – the office of Dr. David Lazan in Vero Beach.
“I didn’t know why this was happening,” she added. “I cried for a whole year. Some days I’d be wrecked. I wouldn’t go to the bathroom for a few days; then I would go up to five times in a single day.”
After a lengthy evaluation and attempt to treat the condition with medication, she was prescribed some physical therapies and pelvic floor muscle exercises. One therapy helped stimulate the bladder with an electric shock, which helped her be able to feel the urgency to go when she needed.
Because of that treatment, she said candidly, “I could realize when I had a full bladder, and then, sit and go.”
She also did a therapy called posterior tibia nerve stimulation, or PTNS, in which a needle is poked into the ankle and sends an electric shock that goes up the nerve in her leg to the bladder.
These two treatments, which she did 10 times each weekly, along with daily pelvic exercise, have almost completely resolved her incontinence. She now only goes once a month for PTNS.
Persistent urinary incontinence can be caused by pregnancy, childbirth, hysterectomy, menopause, obstruction, aging of the bladder muscle, painful bladder syndrome, enlarged prostate, prostate cancer, bladder cancer or bladder stones. Neurological issues such as multiple sclerosis, stroke, Parkinson’s disease, a spinal cord injury and brain tumor can interfere with the nerve signals involved in bladder control.
Fecal incontinence, or bowel incontinence, is the inability to control bowel movements, causing stool to leak unexpectedly. It ranges from occasional leakage to a complete loss of bowel control.
More than half of older Americans struggle with incontinence, according to a recent report by the Centers for Disease Control and Prevention. About half experienced urinary leakage or accidental bowel leakage, and about 25 percent had moderate, severe or very severe urinary leakage. And about 8 percent had moderate, severe or very severe bowel leakage.
“Incontinence is a big health problem and big lifestyle problem,” said Dr. Christopher Tardif, board-certified urologist with Indian River Medical Associates. He says incontinence is a significant problem among many of his patients.
Yet sometimes people are reluctant to come in, or don’t get referred to an urologist, Tardif says, or are worried they may get operated on. But there is a whole spectrum of treatments that can be done, including medications, injections, nerve-stimulating electrodes and various other devices. Physical therapies include pelvic floor muscle exercises to strengthen the urinary sphincter and muscles that control urination.
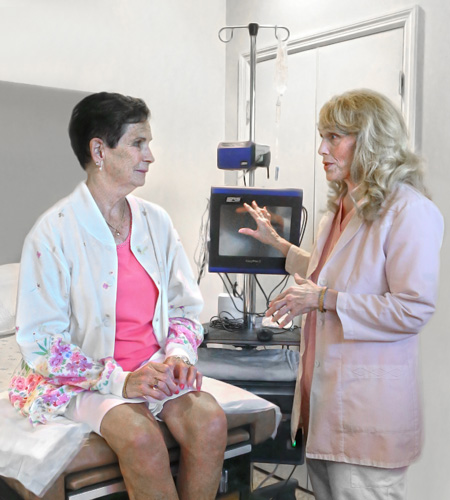
Cindy Gale, a registered nurse in Lazan’s office who is certified in pelvic muscle dysfunction and elimination disorders, helps DiPietro with her physical therapy sessions.
At the pelvic floor rehabilitation center, Lazan’s patients undergo a lengthy evaluation. Diet, exercise and lifestyle are taken into consideration with a treatment plan. The center is a non-surgical facility that promotes the least invasive methods of treating incontinence.
“We help get someone to be able to play cards without getting up 20 times to use the bathroom,” Gale said.
“It’s personal and puzzling to a lot of patients,” she added. “A lot of our patients are older and aren’t used to talking about these kinds of things.”
A sneeze, cough or laugh can trigger leakage.
“It affects where you go, how you go, and where you are in relation to the bathroom,” Gale noted. “Your whole life is geared to being around the bathroom.”
Various behavioral techniques have also proven helpful. Bladder training is done to control urge and other types of incontinence. It involves learning to delay urination after you get the urge to go. The goal is for the person to lengthen the time between trips to the toilet until they’re urinating every two to four hours.
Bladder training may involve double voiding – urinating, then waiting a few minutes and trying again.
Scheduled toilet visits every two to four hours can also be a behavioral technique. In some cases, fluid and diet management can help eliminate the problem.
Several surgical procedures can work well, too, such as sling procedures, bladder neck suspension and artificial urinary sphincter.
And for some, inserting a catheter into the urethra several times a day to drain the bladder is helpful.
“I used to play four hours of golf, go home and cook dinner and then go to the bathroom,” DiPietro lamented.
“I see a lot of women in the pads aisle at the store. A lot of people don’t realize there is something out there they can do.”



