It’s undetectable. It’s deadly. And it presents itself with no warning. A brain aneurysm is like a silent sniper that attacks instantaneously, bursting into a brain bleed that kills half of those afflicted.
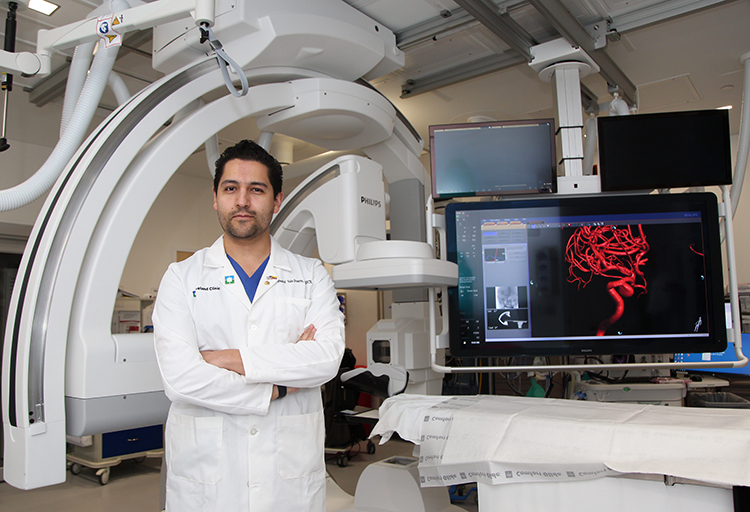
Dr. Daniel Vela-Duarte, a neurologist at Cleveland Clinic Indian River Hospital, is determined to help patients who suffer from brain aneurysms.
“Since there is no test, no blood work or scientific way to determine if someone has an aneurysm, the best-case scenario is that it is found incidentally while undergoing a CAT scan for a headache or other ailment,” he says. “If it is stumbled upon, we can operate and get rid of it before it bursts and causes life-threatening damage.”
A brain aneurysm – also called a cerebra or intracranial aneurysm – is small pouch that grows from a weakened area in the wall of a blood vessel in the brain. As the force of the blood flow in the artery starts hitting that weakened part, that small pouch that becomes like a blister growing over time. If the brain aneurysm expands and the blood vessel wall becomes too thin, the aneurysm will rupture and bleed into the space around the brain.
“The worst-case scenario is when someone comes in with stroke symptoms and the aneurysm has forcefully ruptured and caused a massive brain bleed,” says Dr. Vela-Duarte. “The patient’s awareness and comprehensive abilities are affected, and they may experience weakness on one side of the body. The individual can die very quickly if the artery, specifically where the ruptured pouch occurred, is not repaired in a timely fashion.”
It takes an entire team of physicians and first responders to care for a patient who experiences a ruptured brain aneurysm.
First, recognition of the symptoms by first responders so they can bring the patient to the appropriate medical center with a neuro intravascular interventional surgical center is imperative.
Second, it takes doctors, nurses and other medical professionals with the knowledge to provide effective emergency treatment. Fortunately for Vero Beach residents, Cleveland Clinic’s Indian River Hospital is recognized as a Stroke Center of Excellence and has the equipment and skilled surgeons available to repair the artery.
Finally, post-operative care after surgery plays an important part in the patient’s survival.
“Our mission is to repair arteries in the brain using advanced methods and tools without opening the skull,” Dr. Vela-Duarte explained. “We aren’t doing open surgery but instead we are fixing the arteries and veins, and treating strokes from inside the artery.
“The patient is evaluated by an emergency physician who recommends a CAT scan based on the stroke-like symptoms. If it shows a bleed in a certain area, it is determined whether the bleed is massive or not and if it needs to be drained or not.
“There are a lot of instruments to repair the artery. Utilizing catheters, we insert very small tools that are telescoped inside one another and navigated or threaded through the arterial system until we reach the artery inside the brain to repair the aneurysm.
“Sometimes we enter through the radial artery in your wrist or through the femoral artery in your groin. Once we secure access, we thread a smaller catheter inside the artery all the way up through your abdomen, around the heart and neck and into the skull. We get advanced images of the arteries to visualize the entire map of the arteries and veins hoping to find the aneurysm and treat it.”
According to John Hopkins Medicine, healthcare providers most commonly use coiling to block blood flow into a cerebral aneurysm at risk for rupturing and in some cases may use it to repair a ruptured aneurysm. For endovascular coiling, the catheter is advanced through the artery system to the affected brain artery where the coil is deployed. The coils are made of soft platinum metal and shaped like a spring about the size of a human hair.
“The coil is placed against the entrance or inside the aneurysm to divert the blood flow away from the pouch,” Dr. Vela-Duante said. “The cells around the device create new tissue and down the road the blood should not enter the aneurysm because the device is preventing the blood flow from entering the pouch. This procedure is minimally invasive, and the patient can get the procedure today and go home tomorrow. There is no need for rehab and minimal risk of infection.”
Occasionally, in about 5 percent of the procedures, the artery is so stiff that navigation of the catheter to the brain is not possible. At that point, the procedure will require open surgery.
Dr. Vela-Duante stresses that immediately medical attention is crucial in the case of a brain aneurysm. Symptoms of a ruptured aneurysm mirror those of a stroke, so the same FAST test applies:
F – Face: Ask the person to smile. Does one side of the face droop?
A – Arms: Ask the person to raise both arms. Does one arm drift downward?
S – Speech: Ask the person to repeat a simple phrase. Is the speech slurred or strange?
T – Time: If you see any of these signs call 911 immediately.
“If we can get our community to identify those symptoms and the paramedics to take them to the proper center, we can save more lives,” Dr. Vela-Duante said.
And there are new procedures on the horizon that will enable the neurosurgeon to manipulate the instruments with a robot and navigate the catheters in response to the joy sticks.
There might even be a time before too long when the robot can be operated by a neurosurgeon remotely, providing life-saving access to the procedures at smaller hospitals that don’t have the funds to purchase their own robot or have a full-time neurosurgeon on staff. The world of neurosurgery is constantly evolving and Dr. Vela-Duante seems to be at the forefront.
Dr. Daniel Vela-Duante was recruited by Cleveland Clinic Indian River Hospital two years ago to spearhead their stroke neuro intervascular program. He received his medical degree from Universidad Nacional de Colombia and completed fellowships in neurosurgery at Cleveland Clinic and Baptist Health Neurosurgery/Miami Neuroscience Institute. His office is located at the Health & Wellness Center, 3450 11th Court, Vero Beach. Call 772-563-4741 for an appointment.



