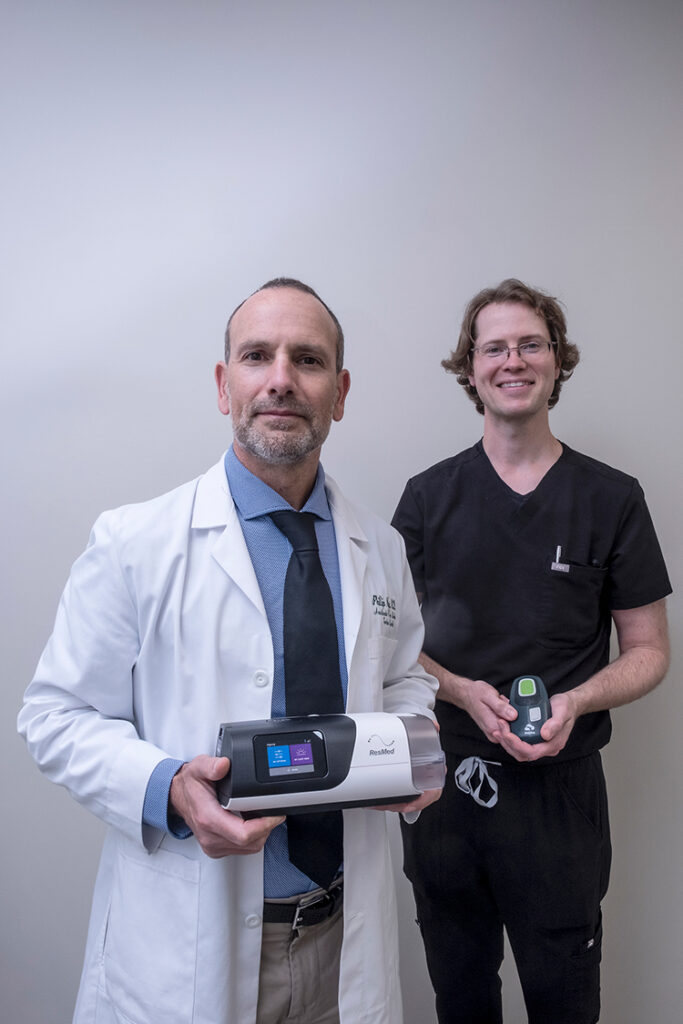
Dr. Timothy Seth Tudor, an ear, nose and throat doctor at Sebastian River Medical Center, is using a hypoglossal nerve stimulator called Inspire to help people with sleep apnea who haven’t had success with other treatments. Inspire, which is manufactured and distributed by Inspire Medical Systems, is the only FDA-approved obstructive sleep apnea treatment that works inside the body to treat the root of cause of sleep apnea with just the click of a button.
As most people know by now, getting a good night’s sleep is paramount to functioning efficiently throughout the day. The leading medical cause of sleep deprivation is obstructive sleep apnea (OSA). OSA occurs when the muscles that support the soft tissues in your throat, such as your tongue and soft palate, temporary relax. When those muscles relax, the airway is narrowed or closed, and breathing is momentarily cut off.
“When the airway closes off the oxidation level goes down, the thorax diaphragm starts to contract and it’s very difficult to breathe,” said Dr. Phillip Nye, a board-certified sleep medicine specialist who collaborates with Dr. Tudor on some cases and refers patients to him. “It’s like a straw with a big piece of fruit stuck in it – you can’t get the liquid through the opening. When that happens, you wake up and as a result of waking up the oxygenation goes low and you get this sympathetic stimulation which is responsible for the fight or flight response. You wake up gasping. People with OSA will do this multiple times a night.”
The gold standard of care and the first line of treatment for OSA is continuous positive airway pressure, otherwise known as CPAP. A CPAP machine uses a hose connected to a mask or nosepiece to deliver constant, steady air pressure to help patients breathe as they sleep.
“CPAP is effective and non-invasive, so we always start there,” Dr. Nye explained. “But roughly 10 percent of people will flat out refuse to use it for whatever reason. Sometimes it has to do with the mask because they feel claustrophobic. Other times they tried it and failed because they just couldn’t wrap their head around being attached to a CPAP device.
“Over the years we looked at other ways to open the airway, focusing on the muscles in the neck right near your larynx, where the windpipe is,” to keep the airway open during sleep.
One solution for patients CPAP hasn’t worked for is the hypoglossal nerve stimulator called Inspire. To be a candidate for treatment you must have moderate to severe obstructive sleep apnea, a body mass index (BMI) lower than 35, and be unable to use or get consistent benefit from CPAP.
“When a patient falls asleep they go into a deep sleep and everything relaxes,” Dr. Tudor explained. “What happens then is the airway collapses at the base of the tongue. With Inspire we can stimulate the branch of the hypoglossal nerve that controls tongue protrusion. When the tongue goes forward it opens up the airway.”
The Inspire device is basically a pacemaker, but instead of stimulating the heart to beat, it stimulates the hypoglossal nerve to help the patient breathe. Every time the device detects an in-breath through built-in sensors, it sends the stimulus to the nerve that controls the tongue to expand the airway. This all happens while the patient remains asleep. The device has a delay feature and does not turn until you are asleep for 15 or 20 minutes. You can pause it when you get up to go to the bathroom, and when you go back to bed there will be another delay as you go back to sleep so that it is not pulsing while you are awake.
“I always do an in-lab sleep study and an endoscopy before surgery to make sure the patient’s airway is collapsing in the way I think it is to determine if Inspire will work,” Dr. Tudor said. “If the patient is a good candidate, then we can proceed with the out-patient procedure done under general anesthesia. The surgery takes about an hour and the patient goes home the same day.”
Inspire is placed under the skin using two small incisions. One incision is made under the chin and second is on the right side of the chest below the collarbone. There’s a little cuff that wraps around the hypoglossal nerve in the neck and a feed that travels under the skin, over the collar bone and down to the battery-operated pulse generator. Inspire is controlled with a small handheld remote that can be adjusted to your sleep patterns.
Approximately 30 days after getting Inspire, you will meet with your doctor to activate the device. Once you and your doctor determine the best settings for you, your doctor will check the status of the device once or twice a year.
“Inspire looks and functions exactly like a pacemaker,” Dr. Tudor said. “It utilizes the same technology for a novel purpose. Eventually the battery will need replacing but that would be a very simple procedure since you don’t have to do the neck incision or the nerve dissection. It’s more of a servicing process and less of an implant.
“Since this procedure has only been done since 2014, we don’t know the exact timing of the battery replacement. We know that a pacemaker lasts five years stimulating 80 times a minute, 24 hours a day, and the Inspire is only stimulating 10-15 times a minute only at night. At that rate, we estimate a battery would last about 10 years.”
Dr. Nye is an anesthesiologist and sleep disorder specialist with a medical degree from Spartan Health Sciences University. He completed his fellowship in sleep medicine at Eastern Virginia Medical School. His practice Neurologic Health and Restorative Sleep is located at 1485 37th Street, Suite 111 in Vero Beach, 772-226-6855.
Dr. Tudor received his medical degree from Oklahoma State University College of Osteopathic Medicine and his residency specializing in Otolaryngology-Head and Neck Surgery at Freeman Health Systems in Missouri. His office is located in Steward Ear Nose and Throat Specialists, 12920 U.S. 1, Suite B, Sebastian, 772-228-9808.