Benign prostatic hyperplasia, (BPH), aside from being a phrase no one would want to draw in a spelling bee, is a medical condition that – sooner or later – affects just about every man on the planet.
The National Kidney & Urological Diseases Information Clearinghouse, (NKUCIC), says BPH affects about half of all men between the ages of 50 and 60 and nearly 80 to 90 percent of men beyond those ages.
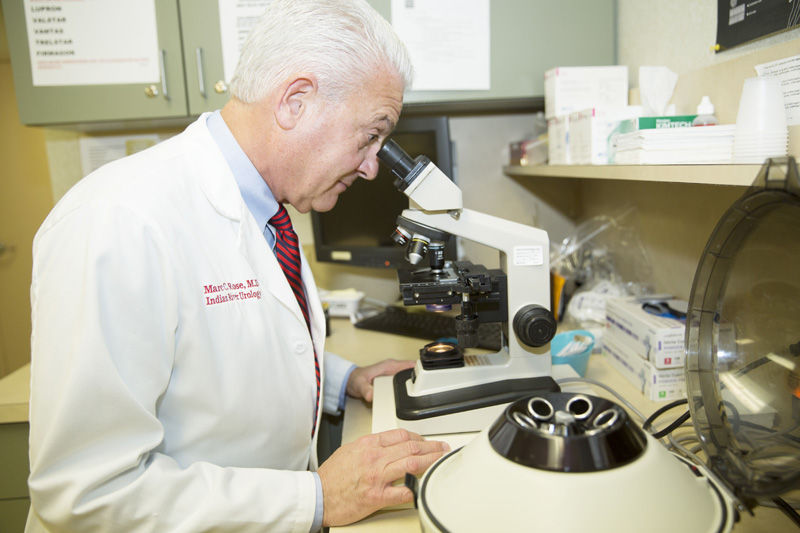
To treat the effects of BPH you could try boiling the bark of an African plum tree for the pygeum chemical it contains that helps alleviate the problem, but a safer and more efficient step would be to meet with an experienced urologist like Dr. Marc Rose at Indian River Urology Associates.
Rose, who first came to Vero in 1986 and partnered with Dr. Hugh McCrystal for 20 years, continues to study and implement the latest advances in urologym, including the recently approved “Urolift” procedure for the treatment of BPH.
In the most basic of terms, BPH is an enlarged, non-cancerous prostate gland. As the prostate grows, it can press up against and pinch the urethra until it very nearly shuts. That pinching or narrowing of the urethra leads to “urinary retention” or the inability to empty the bladder.
According the Urology Care Foundation, that obstruction can bring on a number of symptoms, including the need to urinate frequently (especially at night) in an attempt to empty the bladder, difficulty initiating a urine stream, decreased strength of the urine flow, and dribbling after urination. In severe cases, men with BPH may not be able to urinate at all, which is an emergency that requires immediate attention.
Because BPH is so prevalent in the world’s male population, a variety of treatments have been tried including “natural” remedies such as the above mentioned pygeum from African plum trees along with saw palmetto and rye grass pollen extracts.
Rose, a dyed-in-the-wool Ohio State Buckeye who served his surgical internship and urology residency at Ohio’s world-famous Cleveland Clinic, has an open mind when it comes to such “natural” remedies. “I have patients,” he declares, “who use them and swear by them.” He continues by saying, “There’s no evidence that, for instance, saw palmetto hurts, so I don’t have a problem with patients trying it.”
There are also several pharmaceuticals available including alpha blockers such as terazosin, as well as dutasteride and finasteride, which may help reduce BPH symptoms in many men by blocking the body’s production of a male hormone that causes the prostate to enlarge.
That said, the affable and engaging Rose has an encyclopedic knowledge of surgical techniques he says he knows can help solve BPH problems. The “transurethral resection of the prostate,” or TURP procedure, for instance, removes tissue from the enlarged gland, Rose explains, and has long been considered the “gold standard” in treating BPH.
The somewhat newer and much scarier-sounding “photoselective vaporization of the prostate” or PVP, uses laser energy to vaporize excess prostate tissue, while the “transurethral needle ablation” or TUNA, procedure uses a device inserted through the tip of the penis into the urethra to deliver radio waves that create scar tissue in order to shrink the prostate.
The newest of the new techniques which, Rose, a former lacrosse player cautions, “is not for everyone,” is called the “Urolift system.” There are no radio waves and no cutting, vaporizing, or removal of tissue involved in this procedure, which received FDA approval in October 2013.
Instead, a physician places small, permanent implants into the prostate to lift it off the urethra, which then allows urine to exit the bladder more freely.
There are, however, limits as to who might qualify for this no-cut, no-vaporizing, no-radio wave, no-scarring technique. Chief among them, according to Rose, is the size of the patient’s prostate – in this case, bigger definitely isn’t better.
If the prostate gland has grown too large, or if one of a number of other anomalies exist, Rose warns, this is probably not the procedure to use. That probably helps explain why “not a lot of urologists [are] doing this yet,” according to Rose. He expects the procedure to gain popularity with doctors and patients going forward.
Questions patients can ask their doctor: Is this procedure right for me? What else can I try? What’s the best course of action for my particular situation?
After a physical exam, taking a patient’s history and maybe taking ultra-sound images or using a fiber optic scope, urologists like Rose can radically improve the quality of life for men with BPH.
Losing sleep because of a need to constantly use the restroom in the middle of the night, and other common symptoms of BPH, can quickly become just a memory with proper treatment from an experienced urologist.
Dr. Marc Rose is at Indian River Urology Associates at 787 37th Street, Suite E-200 in Vero Beach. The phone is 772-567-3003.