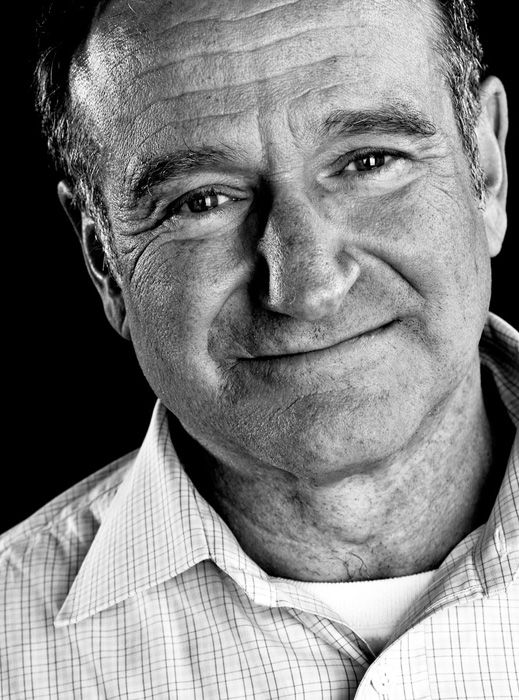
The death of Robin Williams brought chills and sadness to people across the globe. Not only the very fact of his death, but the manner in which it occurred.
Williams’ life ended in suicide. Family members said he had been battling depression, and it was already known he had a history of alcohol addiction.
The link between depression and suicide is undeniable. At least 90 percent of all people who died by suicide in 2011, the most recent year for which statistics are available, were suffering from a mental illness at the time, most often depression, according to the American Foundation for Suicide Prevention.
Some 39,518 suicide deaths were reported in the U.S. that year, making suicide the tenth leading cause of death for Americans.
Just last week after news of Robin Williams’ death, local calls to the 211 Help Line & Crisis Line were up 61 percent, with mental health calls increased as well, according to Patrice Schroeder, public information officer of 211. The hotline serves people on the Treasure Coast.
There are varying degrees of depression from mild to severe. Depression is associated with low levels of certain brain chemicals. These chemicals, which are collectively called neurotransmitters, carry messages between brain cells. Certain neurotransmitters – including serotonin and norepinephrine – are known to affect mood.
“It’s all about the interplay between genetics and perception and internal coping mechanisms,” says Dr. Paul Hebig, board-certified in general psychiatry and forensic psychiatry, and medical director at Indian River Medical Center’s Behavioral Health Center.
Among Americans 45 to 64, depression has jumped more than 30 percent in the last decade, according to the Centers for Disease Control and Prevention. Among white, upper-middle-aged men, the rate has jumped by more than 50 percent, according to the public data.
Among people who are depressed, intense emotional states such as desperation, hopelessness, anxiety or rage increase the risk of suicide. People who are impulsive, or who use alcohol and drugs, are also at higher risk.
One of the things to look for when screening for depression, Hebig says, is a patient’s decrease in interest in activities they once liked to do.
In general, all cases of depression are due to a genetic predisposition for depression, combined with environmental and psychological stressors. In many cases, environmental or psychological stress triggers the genetic expression leading to a depressive episode. Usually a person has a family history of some sort of mood disorder.
Depression spans all ages, genders and races. It is prevalent in children, teens, adults and seniors.
Depression in itself is a clinical diagnosis. It is important to rule out any medical problems that can be leading to a decrease in mood. Something as simple as a thyroid dysfunction can lead to a depressed mood.
“Our perceptions of how someone is doing are different from what their internal perceptions are,” Hebig said. “Their perception of what the environment is offering them may be different from what we see. I would be willing to bet that the public perception of what Robin Williams’ environment had to offer him was quite different than what he saw.”
Spouses and loved ones should be on the notice for any emerging sleep disturbance or any uncharacteristic giving away of possessions, decreased interest in activity and slower thought processes. These are discreet signs, Hebig says.
“Slowly but surely depression is becoming more known as a medical illness, however it still has a somewhat negative stigma to it,” he said, adding that people are somewhat reluctant to seek care.
Part of that reluctance may be due to the fact that oftentimes, depressed people don’t fully appreciate how depressed they are. “Your perceptions do change when you’re depressed,” Hebig said. “You may not see what others see. It’s a tricky illness.”
And it gets even more complicated when there’s a link between depression and substance abuse. The suicide rates are higher in people with mood disorders who do some form of substance abuse, he added.
For someone who has depression and alcohol dependence, the ideal treatment would be medication management plus therapy and participation in a substance abuse program such as Alcoholics Anonymous or even an inpatient substance abuse program.
The good news is that there are a variety of treatment options. Serotonin–norepinephrine reuptake inhibitors (SNRIs) are a class of antidepressant drugs used in the treatment of major depressive disorder and other mood disorders. SNRIs increase the amount of available serotonin and norepinephrine in the brain by blocking the reabsorption of those neurotransmitters.
Therapies that have proven to be effective for some people include electroconvulsive therapy (ECT) – a treatment in which seizures are electrically induced in patients to provide relief from psychiatric illnesses; and transmagnetic (TMS) stimulation – a non-invasive method to cause depolarization or hyperpolarization in the neurons of the brain. TMS uses electromagnetic induction to induce weak electric currents using a rapidly changing magnetic field.
The risks associated with staying on medications are incredibly low versus the risks of not being on them, Hebig said. Some of these medications have shown to have some cardiovascular benefit, or can help prevent the onset of Alzheimer’s disease.
In general, his treatment philosophy is that if a patient has one major depressed episode that gets appropriately treated with medications and has shown a stable mood for an extended period of time, he will attempt to taper that medication off if the patient makes that request.
Yet, if the depression reoccurs, then he’d suggest they stay on the medication indefinitely.
While the medicines are providing benefit in regards to the mood disturbance, hopefully a patient is able to develop a healthier lifestyle, relationship patterns and coping tools.
Kimberly Fuller has been working on coping strategies over the years. The 46-year-old Vero Beach woman was in quiet misery for decades. As a child, she had difficulty getting out of bed some mornings and concentrating in school, and deemed the winters up north where she grew up practically unbearable.
Armed with the antidepressant Zoloft, she fought her depression and went on to marry and have two children. She managed okay until her marriage later disintegrated, sending her into a tailspin, and all-time low in her depression.
“I became extremely sick,” she recalls. “I contemplated taking my life. It was in my head constantly. I’d be driving down the road and think about driving into a ditch.”
“Being depressed feels like you’re stuck,” said Fuller, who has a family history of depression. “For a regular person, the day goes by. When you are depressed, you are so stuck. You look at the clock and only a minute has gone by. The days are long and torturous.”
Fuller, who was eventually diagnosed as bipolar II, otherwise known as manic depression, sought help from Hebig at IRMC where she has had inpatient care for short and long periods of time over the last nine years.
Hebig prescribed electroconvulsive therapy, to which she attributes her “comeback” after being “chronically suicidal.”
In addition to the ECT, she meets with a counselor and case worker to help keep her on a healthy track. Being more stable, she has been able to extend beyond her self-consuming thoughts of troubles and travails, and spend time volunteering for a thrift store that benefits the Family Homeless Center.
“The value of volunteering is huge,” she says. “It has helped my self-esteem. It gets me doing something for someone else. I’m not sitting at home in bed depressed, which doesn’t get you very far.”
She thinks about the late actor/comedian’s fate wistfully. “I wish he had just reached out to someone,” she said. “I know how hard it is. I wish he had just grabbed his wife or picked up the phone. Those bad times come but they don’t necessarily stay. Your life goes through cycles.”
____
211 Help Line & Crisis Line can be reached by dialing 2-1-1 or 1-866-882-2991